Hay Fever
USA
HK - Rhinitis, otherwise known as hay fever, is the most common form of allergy in Hong Kong but whereas in the rest of the world it is caused by pollen and is a seasonal condition, in Hong Kong it is perennial and in the opinion of experts it is triggered by the high level of airborne pollutants.
Japan - wiki : is most commonly caused by pollen from Cryptomeria japonica (known as sugi in Japanese and often incorrectly translated as "cedar") and Japanese cypress (known as hinoki), two native Japanese tree species.
More:
(1)
World Allergy Organization -
There are global differences in the prevalence of seasonal compared to perennial rhinitis.
Climatic differences within continents and countries influence the prevalence of seasonal and perennial rhinitis: perennial rhinitis predominates in coastal regions of Australia, whereas seasonal rhinitis commonly occurs inland.
In general, perennial rhinitis predominates in South America, Asia, Africa and Australia. Perennial and seasonal rhinitis occur commonly in the U.S.A. and Japan. Seasonal rhinitis predominates in Europe.
Worldwide, the allergens most commonly associated with allergic rhinitis are:
(2)
Meet the Pollen Counters (May
5, 2014 7:14 p.m. ET)
- Guy Robinson, a lecturer in natural sciences at
Fordham University, will report the results to the
National Allergy
Bureau, a network of pollen-counting stations.
- Some 30% to 40% of Americans suffer from hay fever.
- For much of the country, cold, wet weather this
spring delayed the onslaught of pollen, but could result in a shorter, albeit
more severe season—what some people are calling a pollen vortex. This has been
the case in places like Atlanta and Denver, where allergy season started later
than usual but has proven to be intense, allergists say.
- People are allergic to different pollens, and it is
common to have reactions to multiple types, experts say. In the spring, trees
generally release pollen first, followed by grass pollen in the late spring and
then weeds, such as ragweed.
- Dr. Robinson isn't making any predictions about
allergy season in the New York area, though he says counts so far have been
low—under 100 pollen particles per cubic meter of air. On one day last week, the
count was just 18. At the height of the season, the numbers can well exceed
1,000.
- Peak tree-pollen counts in the New York area usually
occur when the birch pollen overlaps with the oak.
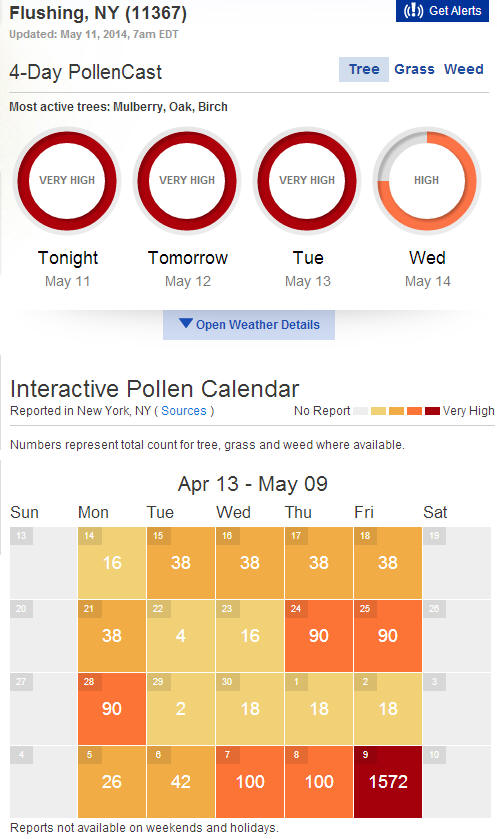
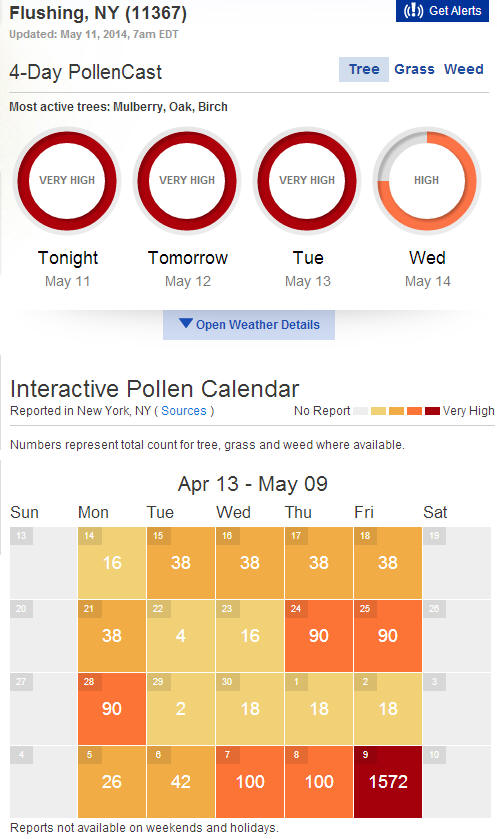
(3) Statistics from weather.com (up to May 11, 2014 - all pollen are from trees; grass has no pollen released yet.)
(4) University of Maryland Medical Center report
- Allergic rhinitis tends to run in families. If one or both parents have allergic rhinitis, there is a high likelihood that their children will also have allergic rhinitis.
- Seasonal allergic rhinitis occurs only during periods of intense airborne pollen or spores.
Grasses. Grasses affect people in mid-May to late June
[in
Maryland]. Grass allergies are experienced more
in the late afternoon.
Tree Pollen. Small pollen grains from certain trees
usually produce symptoms in late March and early April [in
Maryland].
- Other Causes of Chronic Nasal Congestion :
Aging Process. The elderly are at risk for chronic rhinitis
as the mucous membranes become dry with age. In addition, the cartilage
supporting the nasal passages weakens, causing changes in airflow.
- Risk Factors : Allergic rhinitis affects people of all ages. Allergies usually first appear in childhood. Allergic rhinitis is the most common chronic condition in childhood, although it can develop at any age. About 20% of allergic rhinitis cases are due to seasonal allergies, 40% to perennial (chronic) rhinitis, and the rest are mixed.
- Prognosis : Seasonal allergic rhinitis tends to diminish as a person ages. The earlier the symptoms start, the greater the chances for improvement. People who develop seasonal allergic rhinitis in early childhood tend not to have the allergy in adulthood. In some cases, allergies go into remission for years and then return later in life. People who develop allergies after age 20, however, tend to continue to have allergic rhinitis at least into middle age.
- Some evidence suggests that people with allergic rhinitis and asthma may benefit from a diet rich in omega-3 fatty acids (found in fish, almonds, walnuts, pumpkin, and flax seeds) and fruits and vegetables (at least five servings a day). Researchers are also studying probiotics -- so-called good bacteria, such as lactobacillus and bifidobacterium-- which can be obtained in supplements. Some studies have found that probiotics may help reduce allergic rhinitis symptom severity and medication use.
(5) Hay fever affects up to 30% of all people worldwide, including up to 10% of U.S. children under 17 and 7.8% of U.S. adults. The medical cost of allergic rhinitis is approximately $3.4 billion, mostly because of the cost of prescription medications. These figures are probably an underestimate because many of those affected may attribute their discomfort to a chronic cold. Although childhood hay fever tends to be more common, this condition can occur at any age and usually occurs after years of repeated inhalation of allergic substances. The incidence of allergic disease has dramatically increased in the U.S. and other developed countries over recent decades. src
(6) Trends in the epidemiology and prescribing of medication for allergic rhinitis in England.
The age-sex standardized incidence of allergic rhinitis was 5.57 per 1000 person-years in 2001 and increased by 33.0% to 7.41 per 1000 person-years in 2005 (P<0.001). Lifetime age-sex standardized prevalence of a recorded diagnosis of allergic rhinitis increased by 43.2% from 46.35 per 1000 in 2001 to 66.37 per 1000 in 2005 (P<0.001). Over this period a 41.7% overall increase in prescriptions for antihistamines and drugs used in nasal allergy was observed (antihistamines 45.5%, drugs used in nasal allergies 35.5%).
Recorded incidence and lifetime prevalence of allergic rhinitis have increased substantially in recent years. A similar increase in prescriptions for antihistamines and drugs used in nasal allergy in patients with allergic rhinitis is also observed
(7) Allergic rhinitis: definition, epidemiology, pathophysiology, detection, and diagnosis
Allergic rhinitis (AR) is a heterogeneous disorder that despite its high prevalence is often undiagnosed. It is characterized by one or more symptoms including sneezing, itching, nasal congestion, and rhinorrhea. Many causative agents have been linked to AR including pollens, molds, dust mites, and animal dander. Seasonal allergic rhinitis (SAR) is fairly easy to identify because of the rapid and reproducible onset and offset of symptoms in association with pollen exposure. Perennial AR is often more difficult to detect than SAR because of the overlap with sinusitis, respiratory infections, and vasomotor rhinitis. SAR can result in hyperresponsiveness to allergens such as cigarette smoke, once pollen season is over. Perennial AR is defined as occurring during approximately 9 months of the year. AR affects an estimated 20 to 40 million people in the United States alone, and the incidence is increasing; an estimated 20% of cases are SAR; 40% of cases are perennial rhinitis; and 40% of cases are mixed. The pathophysiology of SAR is complex. There is a strong genetic component to the allergic response, which is driven through mucosal infiltration and action on plasma cells, mast cells, and eosinophils. The allergic response occurs in two phases, which are considered the "early" and "late" phase responses. Early phase response occurs within minutes of exposure to the allergen and tends to produce sneezing, itching, and clear rhinorrhea; late phase response occurs 4 to 8 hours after allergen exposure and is characterized by congestion, fatigue, malaise, irritability, and possibly neurocognitive deficits. The key to diagnosis of AR is awareness of signs and symptoms. IgE antibody tests to detect specific allergens are the standard method used today; however, in addition, diagnosis must be confirmed with a positive history and demonstration that the symptoms are the result of IgE-mediated inflammation.
(8) http://www.clevelandclinicmeded.com/
The first recorded case of AR (catarrhus aestivus) was described by Sir John Bostock, who presented himself as a case report to the Medical and Surgical Society of London in 1819.1 At the dawn of the 20th century, there were only several thousand members of the U.S. Ragweed Association. One hundred years later, AR has become the most common allergic/immunologic disorder in the U.S. population,2–4 and now affects an estimated one in seven Americans. AR is acknowledged as a significant health challenge on a global scale.3 AR is a major cause of patient visits to physicians in the U.S., frequently complicates management of other conditions (e.g., asthma, chronic sinusitis), and if untreated or undertreated can lead to considerable morbidity including missed work/school, sleep disruption, diminished daytime performance, and impaired quality of life.2,5 The economic burden of AR is substantial.4
A rising prevalence of AR has been found not only in children,4 but also in adults.5 The peak in incidence of AR occurs during young adult years. Although AR prevalence declines with age, it is also an important health concern in older adults.6 There is an equal incidence of AR in males and females.
Epidemiologic studies have consistently demonstrated that AR and asthma commonly coexist.2 AR is frequently associated with asthma, and is a risk factor for developing asthma; in addition, many patients with AR demonstrate increased bronchial hyperresponsiveness to inhalation challenge with histamine or methacholine.
(9) Google: epidemiology of seasonal allergic rhinitis (SAR)